Role of AI in Theranostics
- Pharma Nuclear Services

- Mar 13, 2023
- 7 min read
Towards Routine Personalized Radiopharmaceutical Therapies
Abstract
We highlight emerging uses of artificial intelligence (AI) in the field of theranostics, focusing on its significant potential to enable routine and reliable personalization of radiopharmaceutical therapies (RPTs). Personalized RPTs require patient-individual dosimetry calculations accompanying therapy. Image-based dosimetry needs: 1) quantitative imaging; 2) co-registration and organ/tumor identification on serial and multimodality images; 3) determination of the time-integrated activity; and 4) absorbed dose determination. AI models that facilitate these steps are reviewed. Additionally we discuss the potential to exploit biological information from diagnostic and therapeutic molecular images to derive biomarkers for absorbed dose and outcome prediction, towards personalization of therapies. We try to motivate the nuclear medicine community to expand and align efforts into making routine and reliable personalization of RPTs a reality.
Introduction
Radiopharmaceutical therapy (RPT) has shown promise in the treatment of various cancer types [1]. Metabolic processes or specific receptors serve as targets for the design of appropriate radiopharmaceuticals. The principle of “theranostics”, in the context of nuclear medicine (Figure 1), uses pairs of radiopharmaceuticals to meet and explore both, therapeutic and diagnostic purposes (i.e. “thera-nostic”). The pharmaceuticals bind to the same target and can be radiolabeled with either a therapeutic (e.g. beta or alpha emitting) or diagnostic imaging (e.g. positron or gamma emitting) radionuclide [2]. This approach allows us to “see what we treat” and “treat what we see” at the molecular level.

Figure 1: An example of the principle of theranostics in nuclear medicine. Here, a radiopharmaceutical (yellow) developed to bind to the target (blue) can be labeled both with Fluorine-18 (18F) for diagnostic imaging purposes and Lutetium-177 for therapeutic procedures.
Two examples of recent radiopharmaceutical developments include targeting (i) the somatostatin receptors for the diagnosis and treatment of neuroendocrine tumors (NET) [3], and (ii) the prostate specific membrane antigen (PSMA) to diagnose and treat metastatic castration resistant prostate cancer (mCRPC) [4]. These are major frontiers in nuclear medicine, with significant existing and upcoming investments and efforts [5]. So far, the procedure guidelines from the International Atomic Energy Agency (IAEA), the Society of Nuclear Medicine and Molecular Imaging (SNMMI), and the European Association of Nuclear Medicine (EANM) have suggested the use of several cycles of a fixed therapeutic injection containing an activity of 7.4 GBq when Lutetium-177 (177Lu) labelled compounds are used for NETs [6] or mCRPC treatments [7]. For NETs, [177Lu]Lu-oxodotreotide has been approved by regulatory agencies to be used with a fixed activity of 7.4 GBq as the only option [8], and a similar framework is expected for [177Lu]Lu-PSMA-617 for mCRPC in the near future.
Treatment planning, however, should consider individual factors such as the patient’s weight and height, the tumor burden, overall patient’s health condition as well as personal preferences and values. The organs at risk (OARs) tolerance to radiation and function as well as the patient-specific biological clearance and uptake of the radiopharmaceutical are further of substantial interest in personalized therapy. The key prerequisite for personalizing RPTs are routine and reliable dosimetry calculations. If dosimetry accompanies RPT, relationships between tumor and OAR radiation absorbed dose and therapy outcomes could be derived, providing evidence for adaptive treatment planning in clinical practice [9].
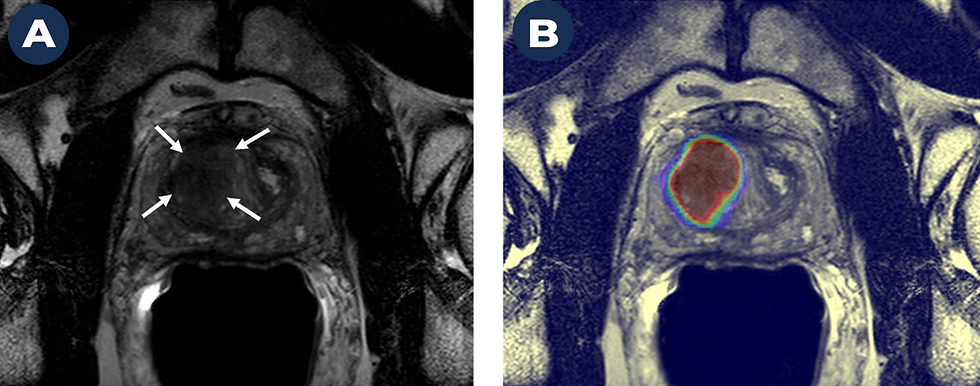
The present state of RPTs (Figure 2A) involves a diagnostic scan that is used by the physician to determine if a patient is suitable for therapy. If the patient expresses the target of interest, it is then referred to several cycles of therapy. Inter-therapy imaging is performed to qualitatively assess the performance of the treatment (e.g. to visualize distribution of the therapeutic radiopharmaceutical). To date, the use of routine post-therapy dosimetry has been hindered by its complexity and immense workload for physicians, technologists, and medical physicists. Thus, to be adopted into routine clinical practice, not only does the technique need to be accurate, but also practical. Any development that simplifies, automates, or accelerates the steps within the dosimetry workflow would be likely to increase implementation of personalized medicine. Artificial intelligence (AI) may be a game changer in supporting and facilitating the dosimetry workflow.

Figure 2: A) Current typical workflow of RPTs in which dosimetry is not routinely implemented. This only requires a diagnostic examination to establish the suitability of a patient for therapy and possibly qualitative images to determine how good or bad the treatment is performing. B) This diagram represents our vision for the whole theranostics approach. AI is a tool that can assist in every step in this workflow. Even more importantly, AI could predict outcomes and absorbed doses from pre-therapy diagnostic scans to personalize the treatment starting from the first cycle.
Our vision for a comprehensive theranostics framework (Figure 2B) involves the use of AI to simplify and motivate the personalization of RPTs. AI not only has direct applications in the different steps that form the dosimetry workflow (Figure 3), but could potentially be used to predict outcomes and absorbed doses.
In this work, we aim to highlight areas of importance on which AI can play a very significant role in dosimetry using the theranostics approach. First, we focus on the current challenges of dosimetry after the administration of the therapeutic radiopharmaceutical and discuss the related AI applications. Later, we describe our
view on how AI can move us towards personalized RPTs making the theranostics workflow proposed in Figure 2B a reality.
Image-based dosimetry in RPTs
The goal of internal dosimetry is to assess the radiation dose absorbed in healthy and malignant tissue. Report 85 of the International Commission on Radiation Units and Measurements (ICRU) [10] defines absorbed dose caused by the interactions of ionizing radiation in organs and tumors as the amount of energy deposited per unit mass of tissue.
The Committee on Medical Internal Radiation Dose (MIRD) has defined guidelines to estimate absorbed dose in RPT using quantitative images acquired at different time points following administration of a therapeutic radiopharmaceutical [11]. These images are used to measure the radiopharmaceutical biodistribution over time [12]. The workflow for image-based dosimetry includes several processing steps [13] that are illustrated in Figure 3 and correspond to the same colored boxes of Figure 2B. Below, we discuss each of the different steps required for accurate absorbed dose assessments and make recommendations on how AI can further assist throughout the workflow.

Figure 3 Schematic representation of the dosimetry workflow for any image-based absorbed dose estimation for radiopharmaceutical therapy.
The role of AI in quantitative imaging
The first step in the dosimetry workflow (Figure 3) is the acquisition of quantitative images that allow for the accurate measurement of activity [14]. The goal is to measure the biodistribution of the radiotracer as a function of time. The number of imaging time points that should be acquired is a compromise between optimization of resources, simplification of protocols, and the accuracy for which the patient-specific effective half-life of the radiopharmaceutical can be estimated [15]. Quantitative imaging also implies the use of standardized acquisition protocols, image reconstruction parameters, and methods to determine the camera calibration factor [11, 16].
Both, single photon emission computed tomography (SPECT) and positron emission tomography (PET), are quantitative imaging modalities that allow us to measure radioactivity distribution in the patient over time. Image acquisition and reconstruction parameters needed for accurate quantification is a topic of ongoing research.
Recent work has assessed the reduction in the number of acquired SPECT projections to reduce scan time without compromising quantitative accuracy or image quality. Rydén et al. [17] used a deep convolutional U-net-shaped neural network to generate intermediate 177Lu SPECT projections (i.e. projections that were not acquired). They found that adding the projections generated by the U-net to the sparsely acquired projections provided similar visual image quality compared to the reference of a full set of projection data. Furthermore, they found comparable kidney activity concentration compared to the one measured from the reconstructed image using a full set of projections. The main advantage of this method is that it allows to scan patients in a much shorter acquisition time. Other investigations have suggested
the reduction in acquisition time per projection or the total number of acquired projections in myocardial perfusion SPECT may be compensated for using a deep residual neural network [18].
AI has also been used to generate quantitative images with PET. Studies involving less injected activity or faster acquisitions have been performed [19-21].
Other studies have focused on improvements in image reconstruction [22-26]. Image degrading effects such as scatter and attenuation need to be corrected for to obtain quantitative images. Scatter correction remains a challenging task in SPECT reconstruction, especially for the imaging of pure-beta emitters that do not create any gamma emissions in their decay chain (e.g. Yttrium-90). In these scenarios, the detected energy spectrum of the photons corresponds to the Bremsstrahlung photons. Xiang et al. [27] used Monte Carlo (MC) simulated phantom data to create projections and understand the scatter components. They used this dataset to train a deep convolutional neural network (CNN) that estimated the scatter component in the projections. The CNN estimated scatter was compared to the one derived from MC simulations. The results were very similar between MC and CNN with the advantage that the latter required only a mere fraction of time compared to MC. The use of a fully connected CNN for SPECT reconstruction was investigated by Shao et al. [28] and outperformed conventional ordered subset expectation maximization (OSEM) SPECT reconstruction in terms of image resolution and quantitation.
In PET, new state-of-the-art reconstruction algorithms such as the block sequential regularized expectation maximization algorithm (BSREM) allow for a higher number of iterations without amplifying the image noise [29]. However, the increased number of iterations also increases the time needed to generate an image. AI has been
used to speed up the reconstruction by generating images for intermediate iterations [30]. The improvements of reconstruction of newly introduced total body PET images using deep learning (DL) methods is subject to ongoing research [31].
Image denoising allows for the reconstruction of quantitative images with less injected activity, faster acquisition times, or with a higher number of iterations in the reconstruction algorithm. There have been studies showing denoising methods using AI CNNs with scintillation cameras data [32], using generative adversarial networks (GAN) [33] for PET, and using coupled U-Nets for SPECT [34].
The interest in targeted alpha therapies [35] is rapidly increasing, though the quantitative imaging remains a challenge [36]. AI methods could be applied to improve both, image quantification accuracy and quality.
To read the article completely , please click on the button below
Source :
Julia Brosch-Lenz, Fereshteh Yousefirizi, Katherine Zukotynski, Jean-Mathieu Beauregard, Vincent Gaudet, Babak Saboury, Arman Rahmim, Carlos Uribe,



Comments